When a benefit file is delivered by ExponentHR to the benefit carrier, the carrier will upload the benefit enrollment election data into their system to ensure they are operating on current information. Upon completion of this process, the benefit carrier may supply a notice to your organization. The carrier notice can vary from something as simple as a confirmation that the file was processed without error, to a request for confirmation of an individual’s enrollment details, or a notice that a particular enrollment does not align with the carrier’s own data or enrollment rules. In the event that additional information or confirmation is needed, the designated individual(s) in your organization will need to respond to the carrier to ensure coverage is being administered accurately to employees.
Note: You must have management access rights to the EDI Utility to use this feature.
To review and respond to carrier notifications:
1. On the Management Navigation Menu, click Communication > EDI UtilityCommunication > EDI Utility.
The EDI UtilityEDI Utility page displays.
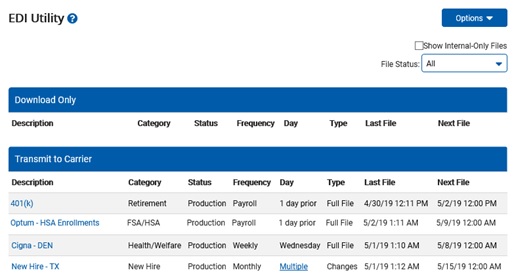
2. The File StatusFile Status drop-down list may be used to filter on files that are currently active (in production), no longer in use (Archived) or currently being developed (Validation Pending).

3. Click on the file description to view EDI File History page for all the system-generated files of the respective benefit plan(s).
Note: The utility displays all applicable files based on transmission type:
Download Only: Files posted for your organization to review and manually deliver to the respective benefit carrier
Transmit to Carrier: Files that are automatically delivered by ExponentHR to the respective benefit carrier
4. Click on the Carrier NoticesCarrier Notices tab of the EDI File History page to access any notifications received by the carrier in response to a delivered file feed are available for your review. The carrier notice can vary from something as simple as a confirmation that the file was processed without error, to a request for confirmation of an individual’s enrollment details, or a notice that a particular enrollment does not align with the carrier’s own data or enrollment rules.

Note: To be actively informed each time a file is generated and/or a carrier response is received, select the Notifications item from the Options drop-down list from the respective EDI File History page. You may also optionally choose which file feeds you want to be actively informed about (when a new file is posted and/or carrier correspondence received) by selecting the Configure Notifications item from the Options drop down menu on the main EDI Utility page.
5. By clicking on the message's subject listed in a specific row, the respective carrier correspondencecarrier correspondence will open for your personal view and reply (if needed).
6. If the selected carrier notice requires a response, you will respond directly to the carrier via email, phone, or through the carrier's message portal.
7. Once addressed, you can indicate that the carrier notice does not need any further attention by using the Status drop-down list to designate the notice as Resolved..
8. Click the Save button.
Related Help Topics:
Understanding Benefit File Feeds
Generating a Non-Scheduled File
Managing Open Enrollment Files
Overriding Enrollment Effective Dates on Benefit File Feed